How Do LPNs Ensure Patient Safety and Infection Control in Healthcare Settings?
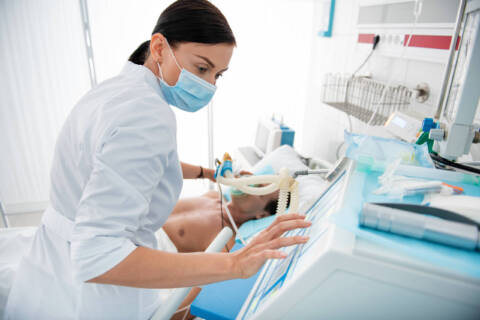
Healthcare settings are crucial for providing effective treatments to sick and recovering patients, but they can also be without proper sanitation measures, especially for susceptible individuals with compromised immune systems. The high volume of sick individuals with contagious illnesses concentrated in hospitals makes them high-risk environments for the spread of viruses and bacteria. Licensed practical nurses (LPNs) are essential in preventing the spread of illnesses in these potentially hazardous settings. Because in-patient nurses interact with their patients multiple times every day, they’re responsible for enacting robust safety measures to protect vulnerable individuals from infection. Bacteria and viruses can remain suspended in the air, elevating the exposure risk of patients, healthcare personnel and visitors, especially in confined healthcare settings. carriers of infections. An indirect microorganism journey, such as a visitor touching a healthcare professional who then goes on to contact vulnerable patients, can have potentially devastating effects on patient safety. dispelled while coughing, sneezing, talking etc. can quickly settle onto nearby surfaces. Laundry, bed rails, sinks, furniture and doorknobs can be fast vehicles for the spread of infections. of all nosocomial bloodstream infections – also known as healthcare-associated infections. Because of the close contact relationship LPNs have with their patients, your education will include focused training on the myriad of health risks susceptible patients face in healthcare settings and how to protect them. As patients’ first line of defense against infections, LPNs must adhere to strict sanitation protocols, including thorough hand hygiene. Thoroughly washing your hands before and after patient contact or after handling contaminated items is crucial to protect the well-being of other patients and yourself. Personal Protective Equipment (PPE) – gloves, masks, gowns and eyewear – are another key component of LPNs’ duty to their patients. Their ability to assess when PPE is required, and which type is needed to lower the possibility of patient infection, is an essential aspect of their day-to-day job. LPNs need to ensure a patient’s room is safe to reside in. Regularly cleaning, disinfecting and sterilizing equipment and surfaces is integral to maintaining a clean environment for patients to effectively recover. You also need to stay vigilant about how medical devices – such as catheters – are stored and utilized, as improper handling can increase your patient’s risk of nosocomial infection. As an LPN, you’ll be required to educate patients and their families about hand hygiene and PPE as well as how to recognize signs of infections in themselves. Even a well-meaning family member can infect the patient if they don’t adopt proper safety measures. At St. Louis College, we provide a rigorous education that thoroughly prepares students to become LPNs, and LPNs to become RNs (registered nurses). With our , you can become eligible for higher and better-paying managerial positions with an advanced degree. Our experienced staff and rigorous curriculum – including hands-on clinical training – will enhance your diagnostic and implementation abilities, giving you the confidence to perform optimally in your duties. To learn more about how you can position yourself in your dream healthcare career, or call 866-529-2070 today.