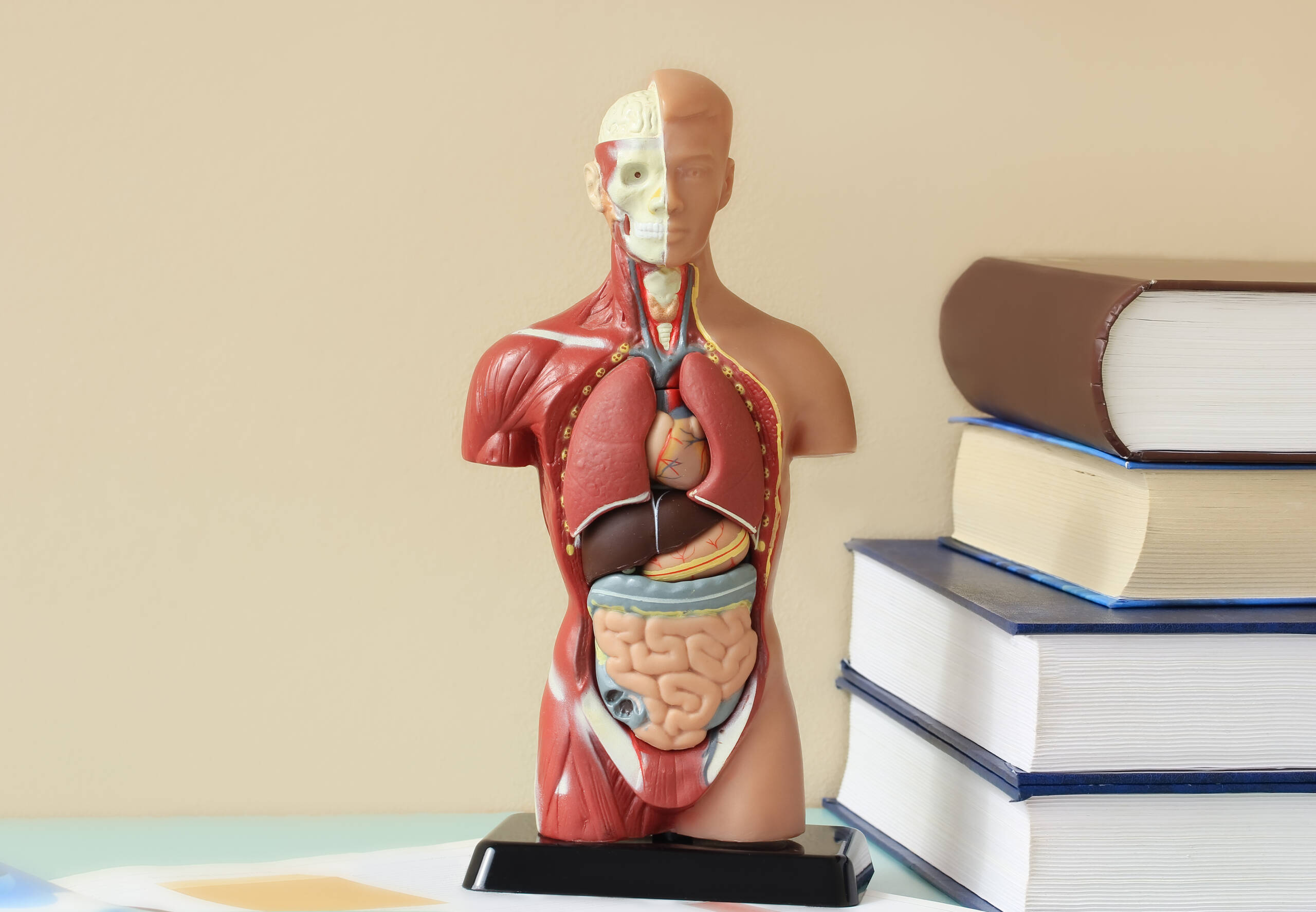
Understanding Human Biology is Important for Healthcare Careers
Understanding human biology is fundamental to having a successful healthcare career. Whether you aspire to become a doctor, nurse, physical therapist or medical assistant, you won’t be able to earn a degree without showing competency in your chosen field. Having at least a basic knowledge of human biology may help you more easily grasp diagnostic and treatment concepts that will be relevant in your education and ultimately enable you to make more informed decisions that keep your patients safe. The good news is you don’t have to major in human biology if you want to work in the healthcare field, especially if you’re not particularly interested in spending the better part of a decade pursuing a doctorate. For instance, if your goal is to become a physical therapy assistant, you can enroll in an associate-degree PTA program with coursework focused on aspects of human biology relevant to your profession, such as human anatomy and physiology. Human biology is a branch of biology that is focused on the scientific study of the human organism. Studying human biology sheds light on how our bodies work, how they’ve evolved over time and how we interact with our physical environment. Some medical professionals, especially doctors, need to have a deep and comprehensive understanding of human biology, however those pursuing more focused roles in the medical field like phlebotomy or physical and occupational therapy usually only need to focus on certain aspects of the discipline relevant to their profession. All of these systems work together to ensure the human body works correctly and keeps various diseases and medical conditions at bay. A respiratory therapist works under the supervision of a doctor and treats patients who are having trouble breathing. Their duties include giving patients oxygen, managing ventilators and administering medication to the lungs. To become a respiratory therapist, students must learn different aspects of human biology, with an emphasis on the respiratory and cardiovascular systems. A phlebotomist’s primary job is to draw blood from patients and send it off to medical labs for testing. Most phlebotomy programs include coursework which focuses on exploring the lymphatic and cardiovascular systems. A physical therapy assistant works under the supervision of a physical therapist and treats patients through exercise, massage and stretching. To become a physical therapy assistant, you’ll need to have an in-depth understanding of the skeletal and muscular systems. An occupational therapy assistant works under the supervision of an occupational therapist helping patients regain or develop the ability to perform everyday tasks, such as eating, getting dressed and bathing. Similar to a physical therapy assistant, an occupational therapy assistant must study the skeletal and muscular systems, but also the nervous system. If you’re looking to leap into the ever-growing and ever-evolving field of healthcare, but you’re not sure which career is right for you, consider studying at the St. Louis College of Health Careers. We offer a variety of accredited and flexible that allow you to work at your own pace and gain valuable hands-on experience without spending years in school. Browse the opportunities we offer and reach out to us with any questions you may have by calling 866-529-2070.
Details